Warning:This article contains information about eating disorders and disordered eating.
When you think of a person with an eating disorder, what shape and age comes to mind?
We often think of young females with model-type bodies suffering from either Anorexia Nervosa or Bulimia Nervosa. Would you believe that is only a small percentage of the population that suffers from eating disorders?
In the military community, service members and veterans are more likely to engage in disordered eating patterns than civilians. The true percentage of service members and dependents with clinical eating disorders is unknown because of the lack of support in appropriate eating disorder (ED) recovery, and the confusion behind disordered eating (which looks a lot like praise). Many studies cite that eating disorders are used as a coping strategy in the military community.
The Difference in Eating Disorders and Disordered Eating
Eating disorders are clinically diagnosed with very specific guidelines in the Diagnostic and Statistical Manual 5th Edition-Text Revision (DSM 5-TR). These include Anorexia Nervosa, Bulimia Nervosa, and binge eating. Although Orthorexia Nervosa is not officially recognized in the DSM 5-TR, many mental health professionals recognize the harmful components on both the physical and mental health of patients. Orthorexia has been on the rise in recent years due to the marketing of “clean eating,” but it is difficult to acknowledge and diagnose because it can be confused with Other Specified Eating Disorder (OSFED) or Avoidant Restrictive Food Intake Disorder (ARFID).
Disordered eating is a much murkier discussion because it is a list of potential symptoms that can potentially escalate an eating disorder. The symptoms promote an unhealthy relationship with food, exercise, and body image. These may be behaviors like: avoiding food as punishment for overeating, assigning morality to foods (organic food is “good,” and processed food is “bad”), increasing or over-exercising as punishment for skipping a workout, throwing away food to avoid binging on it, yo-yo dieting and yo-yo weight loss, use of cleanses or laxatives, just to name a few. The scariest part about disordered eating: it’s widely praised and accepted as part of fitness and wellness culture. It is seen as “healthy” and “disciplined.” Existing in a larger body is widely stigmatized, and in part why larger bodied individuals are overlooked for potential eating disorder diagnoses or receiving appropriate medical attention for disordered eating.
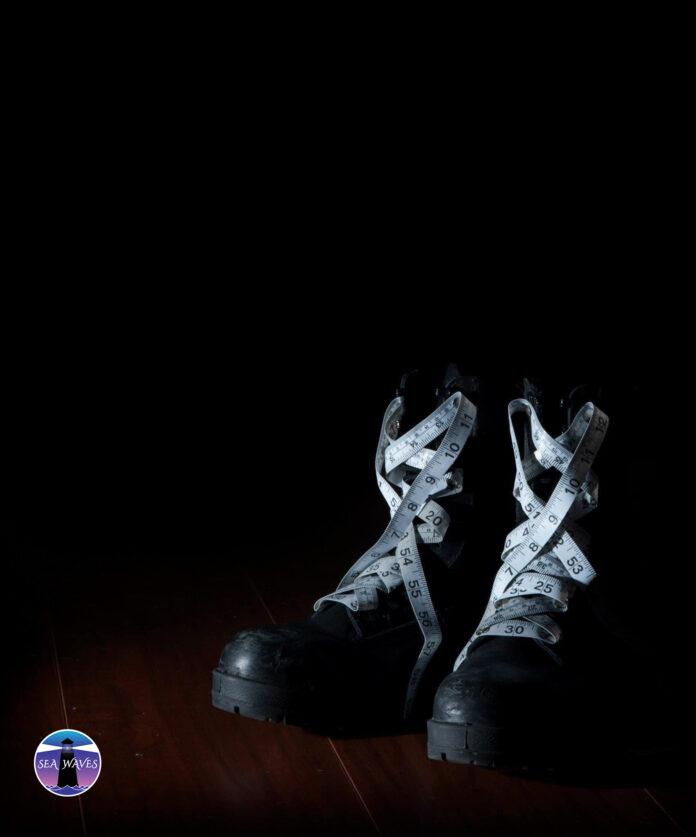
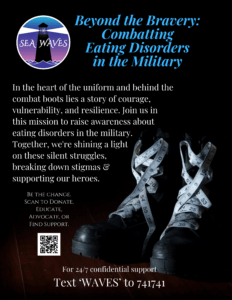
The Sea Waves Mission
I had the opportunity to speak with Leah Stiles back in February of this year about her non-profit organization, Sea Waves. Leah is a retired sailor who is one of many military service members that suffered from an eating disorder and did not receive appropriate support in recovery. Leah explains that as she went higher in rank, the more her eating disorder spiraled, and the more she was praised by her sailors and superiors for being “in shape.” Ask anyone recovering from an eating disorder how confusing that type of messaging is: on the inside you are wasting away, and on the outside everyone is praising you for existing in a smaller body.

After retiring from the Navy as a Senior Chief Mass Communication Specialist, Leah Stiles chose to help those like her who were struggling with eating disorders, and founded the nonprofit, Sea Waves. The goal of Sea Waves is to provide eating disorder support for military service members and their dependents. What makes this such a daunting task? There is currently limited accurate data on how many service members are suffering from an eating disorder or are in eating disorder recovery. The DOD has yet to formally acknowledge that they do not have the appropriate resources in place to support service members or their dependents with active eating disorders or play a role in disordered eating prevention. There is limited appropriate support for referrals at the primary care level. To add, there are not enough behavioral health professionals or registered dietitians who are properly trained to support those in active eating disorders, those recovering, or those struggling with disordered eating. I was even more shocked to learn that the cost of in-patient eating disorder treatment for Tricare beneficiaries stops at age 20. This confirms the notion that eating disorders are stigmatized to adolescents, they are something that one simply “grows out of.”
But People in the Military Are Supposed to be Fit!
Military recruitment advertises a sense of stability that service members and their dependents may not have had experienced before; especially when it comes to food security and free support for fitness and nutrition programs as well as behavioral health services. With so many voices about what is “healthy,” “fit,” and “self discipled,” it is very easy to find that you are drowning in misinformation that will leave you more than malnourished.

Being in the military does require a standard level of fitness to be able to support the mission. There are also many programs that support nutrition education, evidence based postpartum recovery for female service members, and weight maintenance. The issue? There is little to no training among these professionals to appropriately support service members or dependents showing signs of disordered eating or in an active eating disorder both on the civilian and DOD sides of medicine. In fact a study in 2017 indicated that 49% of registered dietitians in the US shows signs of Orthorexia Nervosa (PMID: 28624376) while an unknown percentage of fitness coaches suffer from disordered eating tendencies themselves. Fatphobia is a term that is defined as a fear of fatness. This is especially dangerous in a medical setting where staff can discriminate or potentially neglect the health concerns of larger bodied individuals- focusing solely on their weight as the cause of any and all health problems. Not only does this lead to malpractice, but causes patients to neglect their health out of fear of shame. If this is happening in military treatment facilities all over the world, how can our service members recover and continue their service? How can their spouses or children heal and make peace with their bodies?
It is also important to mention here to those that think: “eating disorders weren’t a problem in MY military!” they likely were a problem. Much like mental health progress, the stigma around admitting that one had an eating disorder was too great and accessing appropriate treatment was too limited. Let’s remember that not long ago, lobotomies were considered appropriate treatment for PPD.
Refuse to Shrink- Get Involved!
So what can we do while policy and support lags behind? Even when the day comes that active service members receive appropriate support for eating disorders or their disordered eating, the support for veterans and dependents may take longer. We must first re-define the cultural expectation that small bodies are more worthy. Much like the opioid addiction crisis, eating disorders do not discriminate: no religion, gender, level of education, race, socioeconomic status, or body is safe from developing an eating disorder. Once you identify that small folks, even in poor health, are praised for being …small, it is easy to spot misleading and predatory tactics used by the fitness, diet, and wellness industries that influence our choices about how we care for our bodies. In a sub culture that encourages “making weight at all costs,” disordered eating can spiral very quickly and cause additional health concerns. If you feel that you are experiencing disordered eating symptoms, speak with your primary healthcare provider and request they refer you to a therapist that has experience in body image and disordered eating support.
You can join the Sea Waves mission in many different ways. This is a non profit, so making waves by means of financial support is of the utmost importance to changing policy to support service members, their dependents, and veterans. Sea Waves has also partnered with our dear friend Erin, owner of The Dainty Forces, to create a bracelet titled: “Refuse to Shrink.” 10% of proceeds are returned to Sea Waves with each purchase of this bracelet. You can find and follow Sea Waves on Instagram, and become a newsletter subscriber through their website. Sea Waves utilizes volunteer opportunities in highly populated military locations and welcomes volunteers from all walks of life. They have both local and digital volunteering options based on your available level of commitment. Finally, if you have read this article and realized that you need to get help for your disordered eating or an active eating disorder, you can text “WAVES” to 741741 to receive 24/7 confidential support for free.
Make waves of change. Refuse to shrink!










Great Article Taylor!
Comments are closed.